All about the skin around the eyes and “drooping” eyelids
04/04/2025

16/03/2023
Glaucoma is a chronic irreversible optic nerve disease due to many reasons, the most important risk factor of which is high intraocular pressure (IOP).
We speak of glaucoma when we find that the optic nerve, which acts as a conductor of information from the eye to the brain, is affected. IOP is determined by the production of aqueous humour (the liquid responsible for the eye's tone) and the resistance and difficulty involved in its drainage.
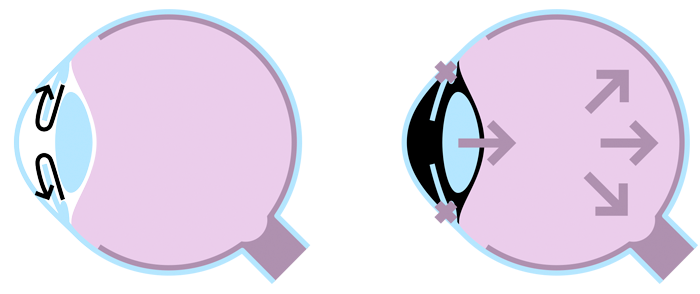
On the left, an illustration of a healthy eye. Correct drainage. Normal intraocular pressure. On the right, an illustration of an eye with glaucoma. High intraocular pressure due to resistance and difficulty in draining the aqueous humour.
There is a wide variety of types of glaucoma although in general terms we can classify them according to their origin (primary and secondary) and angle width (open- or closed-angle).
The majority of those affected do not usually show symptoms until the advanced stages of the diseases, when the patient has tunnel vision.
This happens because of a loss of lateral vision, which the patient does not notice because the brain has the ability to compensate for the lost vision and fill in the blind spots by combining the images in both eyes to give a complete image.
This is why it is called 'the silent thief' and early detection is crucial.
Diagnosis is vitally important and it can be done with an IOP measurement, with the visual field or with an optical coherence tomography (OCT).
There are risk factors for the appearance of glaucoma.
In addition, there are factors that may condition the progression of glaucoma
The majority of treatments are aimed at increasing drainage and, in some case, reducing the production of aqueous humour. From least to more invasive treatments, we find medical-drug treatments, outpatient laser treatment and surgery.
Early detection and timely treatment significantly improve the visual prognosis of the disease and can prevent progression to blindness.
Dr. Jesús Téllez, ophthalmologist at the Barraquer Ophthalmology Centre